
The confusion stemming from the face mask mandates around the world seem to stem from a lack of clinical information easily available to the public, as opposed to what the public are given by the corporate and government sponsored media. While some studies are indeed cited here and there, one of the most informative organizations for compiling all of the research comes from the Swiss Policy Research. We encourage readers to go the their website and click on their source links to unravel the information themselves. Happy enlightening!
1. Studies on the effectiveness of face masks
So far, most studies found little to no evidence for the effectiveness of cloth face masks in the general population, neither as personal protective equipment nor as a source control.
A May 2020 meta-study on pandemic influenza published by the US CDC found that face masks had no effect, neither as personal protective equipment nor as a source control. (Source)
A July 2020 review by the Oxford Centre for Evidence-Based Medince found that there is no evidence for the effectiveness of cloth masks against virus infection or transmission. (Source)
A Covid-19 cross-country study by the University of East Anglia found that a mask requirement was of no benefit and could even increase the risk of infection. (Source)
An April 2020 review by two US professors in respiratory and infectious disease from the University of Illinois concluded that face masks have no effect in everyday life, neither as self-protection nor to protect third parties (so-called source control). (Source)
An article in the New England Journal of Medicine from May 2020 came to the conclusion that cloth face masks offer little to no protection in everyday life. (Source)
An April 2020 Cochrane review (preprint) found that face masks didn’t reduce influenza-like illness (ILI) cases, neither in the general population nor in health care workers. (Source)
An April 2020 review by the Norwich School of Medicine (preprint) found that “the evidence is not sufficiently strong to support widespread use of facemasks”, but supports the use of masks by “particularly vulnerable individuals when in transient higher risk situations.” (Source)
A July 2020 study by Japanese researchers found that cloth masks “offer zero protection against coronavirus” due to their large pore size and generally poor fit. (Source)
A 2015 study in the British Medical Journal BMJ Open found that cloth masks were penetrated by 97% of particles and may increase infection risk by retaining moisture or repeated use. (Source)
An August 2020 review by a German professor in virology, epidemiology and hygiene found that there is no evidence for the effectiveness of cloth face masks and that the improper daily use of masks by the public may in fact lead to an increase in infections. (Source)
Additional aspects
There is increasing evidence that the SARS-2 coronavirus is transmitted, at least in indoor settings, not only by droplets but also by smaller aerosols. However, due to their large pore size and poor fit, cloth masks cannot filter out aerosols (see video analysis below): over 90% of aerosols penetrate or bypass the mask and fill a medium-sized room within minutes.
The WHO admitted to the BBC that its June 2020 mask policy update was due not to new evidence but “political lobbying”: “We had been told by various sources WHO committee reviewing the evidence had not backed masks but they recommended them due to political lobbying. This point was put to WHO who did not deny.” (D. Cohen, BBC Medical Corresponent).
An analysis by the US CDC found that 85% of people infected with the new coronavirus reported wearing a mask “always” (70.6%) or “often” (14.4%). Compared to the control group of uninfected people, always wearing a mask did not reduce the risk of infection.
Japan, despite its widespread use of face masks, experienced its most recent influenza epidemic with more than 5 million people falling ill just one year ago, in January and February 2019. However, unlike SARS-CoV-2, the influenza virus is easily transmitted by children, too.
Many states that introduced mandatory face masks on public transport and in shops in spring, such as Hawaii, California, Argentina, Spain, France, Japan and Israel, saw a strong increase in infections from July onwards, indicating a low effectiveness of mask policies. (More examples)
Austrian scientists found that the introduction, retraction and re-introduction of a face mask mandate in Austria had no influence on the coronavirus infection rate.
In the US state of Kansas, the 90 counties without mask mandates had lower coronavirus infection rates than the 15 counties with mask mandates. To hide this fact, the Kansas health department tried to manipulate the official statistics and data presentation.
Contrary to common belief, studies in hospitals found that the wearing of a medical mask by surgeons during operations didn’t reduce post-operative bacterial wound infections in patients.
During the notorious 1918 influenza pandemic, the use of cloth face masks among the general population was widespread and in some places mandatory, but they made no difference.
Asian countries with low covid infection and death rates benefited not from face masks but mainly from early border closures. This is confirmed by Scandinavian countries like Norway, Finland and Denmark, which didn’t introduce mask mandates but closed borders early and saw very low covid infection and death rates, too.
Development of cases after mask mandates
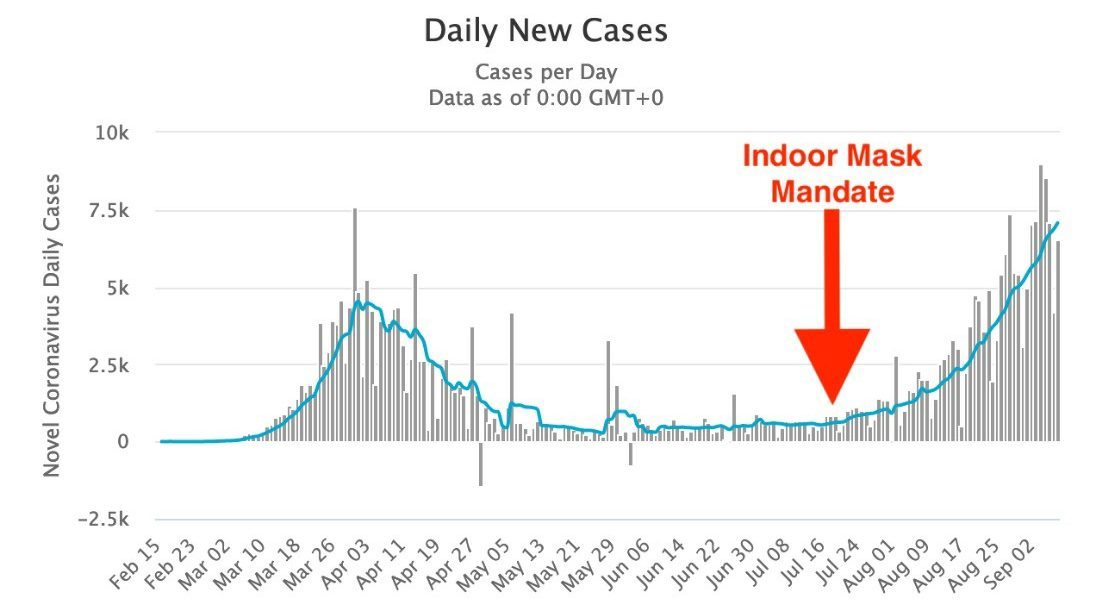
In many states, infections began to increase after mask mandates were introduced. The following chart shows the very typical example of France. Other examples include California, Florida, Hawaii, Argentina, Peru, the Philippines, Spain, France, the UK, Israel, Japan, Switzerland and many more.
Some recent studies argued that cloth face masks are indeed effective against the new coronavirus and could at least prevent the infection of other people. However, most of these studies suffer from poor methodology and sometimes show the opposite of what they claim.
Typically, these studies ignore the effect of other measures, the natural development of infection numbers, changes in test activity, or they compare countries with very different conditions.
An overview:
A meta-study in the journal Lancet, commissioned by the WHO, claimed that masks “could” lead to a reduction in the risk of infection, but the studies considered mainly N95 respirators in a hospital setting, not cloth masks in a community setting, the strength of the evidence was reported as “low”, and experts found numerous flaws in the study. Professor Peter Jueni, epidemiologist at the University of Toronto, called the WHO study “essentially useless”.
A study in the journal PNAS claimed that masks had led to a decrease in infections in three global hotspots (including New York City), but the study did not take into account the natural decrease in infections and other simultaneous measures. The study was so flawed that over 40 scientists recommended that the study be withdrawn.
A German study claimed that the introduction of mandatory face masks in German cities had led to a decrease in infections. But the data does not support this claim: in some cities there was no change, in others a decrease, in others an increase in infections (see graph below). The city of Jena was an ‘exception’ only because it simultaneously introduced the strictest quarantine rules in Germany, but the study did not mention this.
A US study claimed that mandatory masks had led to a decrease in infections in 15 states, but the study did not take into account that the infection rate was already declining in most states at that time, and a comparison with other states was not made. After the study was published, infections began to increase in states with mask mandates (e.g. in California, Florida and Hawaii).
A Canadian study claimed that countries with mandatory masks had fewer deaths than countries without mandatory masks. But the study compared African, Latin American, Asian and Eastern European countries with very different infection rates and population structures.
A small review by the University of Oxford claimed that face masks are effective, but it was based on studies about SARS-1 and in health care settings, not in community settings.

Wearing masks for a prolonged period of time is not harmless, as the following evidence shows:
The WHO warns of various “side effects” such as difficulty breathing and skin rashes.
Tests conducted by the University Hospital of Leipzig in Germany have shown that face masks significantly reduce the resilience and performance of healthy adults.
A German psychological study with about 1000 participants found “severe psychosocial consequences” due to the introduction of mandatory face masks in Germany.
The Hamburg Environmental Institute warned of the inhalation of chlorine compounds in polyester masks as well as problems in connection with face mask disposal.
The European rapid alert system RAPEX has already recalled 70 mask models because they did not meet EU quality standards and could lead to “serious risks”.
In Germany, two 13-year-old children died suddenly while wearing a mask for a prolonged period of time; autopsies couldn’t exclude CO2 intoxication or a sudden cardiac arrest.
In China, several children who had to wear a mask during sports classes fainted and died; the autopsies found a sudden cardiac arrest as the probable cause of death.
In the US, a car driver wearing an N95 (FFP2) mask fainted and crashed into a pole.
Conclusion
Cloth face masks in the general population might be effective, at least in some circumstances, but there is currently little to no evidence supporting this proposition. If the SARS-2 virus is indeed transmitted via indoor aerosols, cloth masks are unlikely to be protective. Health authorities should therefore not assume or suggest that cloth face masks will reduce the rate or risk of infection.
See also
Facts about Covid-19
Studies on Covid-19 lethality
On the treatment of Covid-19
